Yes! Taking active control of your sexual health starts with open communication with your provider.
There are many other steps you can take to protect your sexual health this summer, such as routine testing for STIs, including HIV, seeking HIV PrEP, and doxy-PEP.
Visit SFCityClinic.org for more information or call to schedule an appointment.
You can also schedule an appointment with your medical provider to discuss how you can stay active in your sexual health routine.
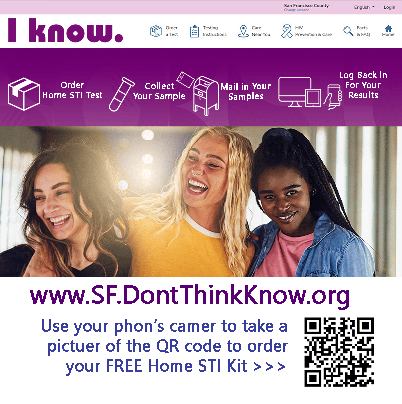
You can also get tested for STI's and HIV at home by ordering a test kit from take-me-home.org.
Cases of mpox are still occurring. If you have not been vaccinated, get vaccinated, which includes making time for both shots. If you only got the first one, you can still get the second.
Having both shots offers you the strongest protection.
Speak to your medical provider about getting yours today.
Visit SF.gov/mpox for more mpox information or visit us online at www.SFCityClinic.org or call 628-217-6600 to schedule an appointment for the mpox vaccination at San Francisco City Clinic.